The evaluation of pediatric airway anatomy and dynamics continues to evolve with the development of newer technologies. While endoscopic procedures remain the gold standard for direct visualization of the airway, radiographic advances allow providers to perform less-invasive initial testing or complementary imaging to help guide diagnosis and treatment plans. Current methods for localizing obstruction in pediatric airway disease include plain radiographs, cinematic MRI (C-MRI), CT scans, and virtual endoscopy (VE).
Plain radiographs are most helpful to evaluate acute upper airway obstruction and may help locate foreign bodies. Lateral neck radiographs may be used as an initial screening tool to evaluate for adenoid hypertrophy and visualize the nasopharyngeal airspace and retropharyngeal soft tissue in patients with chronic symptoms of upper airway obstruction. Plain radiography is fast, inexpensive, and accessible; though, it provides significantly less detail compared with laryngoscopy and other advanced imaging techniques.1
C-MRI provides high-resolution imaging of soft tissues without ionizing radiation and can be especially beneficial in identifying lymphoid tissue hypertrophy and multisite airway compression in patients with OSA. Given the length of time needed to complete the study, procedural sedation is usually needed in the pediatric population. When compared with drug-induced sleep endoscopy, endoscopy was shown to be superior in examining nasal and supraglottic obstruction, as well as more sensitive to partial collapse of the airway. These techniques prove to be most helpful in tandem to one another.2
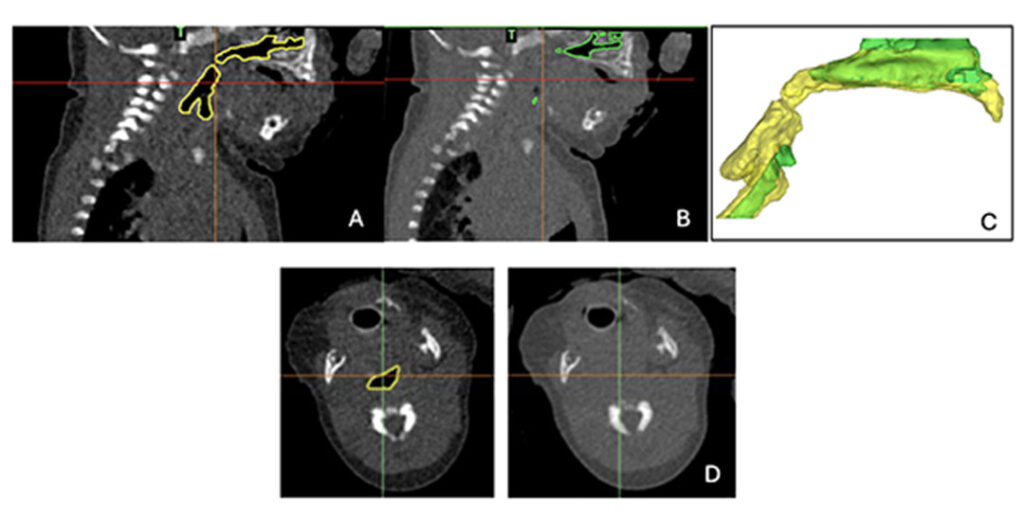
A CT scan of the chest is one of the most widely available and commonly used methods to evaluate the pediatric lower airway, offering a fast radiographic technique that provides detailed views of the airway, surrounding submucosal tissue, and vasculature without the requirement of sedation. Post-processing of CT scan images led to the creation of VE. While remaining an ongoing area of research, studies have demonstrated that VE is comparable with direct endoscopy in identifying and measuring fixed airway lesions but less sensitive in identifying dynamic airway changes.3,4 A newer variation of a CT scan, dynamic volumetric CT scan, has demonstrated usefulness in identifying tracheobronchomalacia in pediatric patients.5–7 This test is performed with free breathing and utilizes a relatively low amount of radiation. Figure 1 demonstrates how this imaging modality may also prove to be beneficial in identifying and quantifying hypopharyngeal collapse in addition to lower airway collapse in infants.
The ability to localize the type (dynamic vs fixed) and specific area of obstruction, particularly in pediatric patients with chronic respiratory failure or OSA, is crucial to surgical planning and ongoing medical management. Therapy can be tailored using a combination of both radiographic and procedural techniques. Multiple factors impact whether providers perform advanced imaging and/or procedures as a part of an initial airway evaluation, including the safety of procedural sedation, cost burden, availability of imaging and/or proceduralists, parental preference, and institutional preferences and biases. Further comparative studies are needed amongst the newest radiographic techniques and procedures to determine a more universal, streamlined approach to evaluate pediatric patients with airway obstruction.
References
1. Walner DL, Donnelly LF, Ouanounou S, Cotton RT. Utility of radiographs in the evaluation of pediatric upper airway obstruction. Ann Otol Rhinol Laryngol. 1999;108(4):378-383. doi:10.1177/000348949910800411
2. Li C, Kou YF, DeMarcantonio MA, et al. Sleep endoscopy and cine magnetic resonance imaging evaluation of children with persistent obstructive sleep apnea. Otolaryngol Head Neck Surg. 2023;168(4):848-855. doi:10.1177/01945998221097659
3. Burke AJ, Vining DJ, McGuirt Jr., WF, Postma G, Browne JD. Evaluation of airway obstruction using virtual endoscopy†. Laryngoscope. 2000;110:(1):23-29. doi: 10.1097/00005537-200001000-00005
4. Men S, Ecevit MC, Topçu I, Kabakçi N, Erdağ TK, Sütay S. Diagnostic contribution of virtual endoscopy in diseases of the upper airways. J Digit Imaging. 2007;20(1):67-71. doi:10.1007/s10278-006-0857-4
5. Koenigs M, Young C, Lillis A, et al. Dynamic volumetric computed tomography angiography is an effective method to evaluate tracheomalacia in children. Laryngoscope. 2023;133(2):410-416. doi:10.1002/lary.30125
6. Pugh CP, Ali S, Agarwal A, Matlock DN, Sharma M. Dynamic computed tomography for evaluation of tracheobronchomalacia in premature infants with bronchopulmonary dysplasia. Pediatr Pulmonol. 2023;58(11):3255-3263. doi:10.1002/ppul.26652
7. Ngerncham M, Lee EY, Zurakowski D, Tracy DA, Jennings R. Tracheobronchomalacia in pediatric patients with esophageal atresia: comparison of diagnostic laryngoscopy/bronchoscopy and dynamic airway multidetector computed tomography. J Pediatr Surg. 2015;50(3):402-407. doi:10.1016/j.jpedsurg.2014.08.021