
Mechanical ventilation is a lifesaving therapy for patients with ARDS. However, it is well known that mechanical ventilation itself can contribute to ventilator-induced lung injury (VILI).1 VILI may occur due to alveolar overdistention (volutrauma), excessive airway pressure (barotrauma), repetitive alveolar collapse and reopening (atelectotrauma), or the cumulative energy delivered to the lungs—referred to as mechanical power.1–4
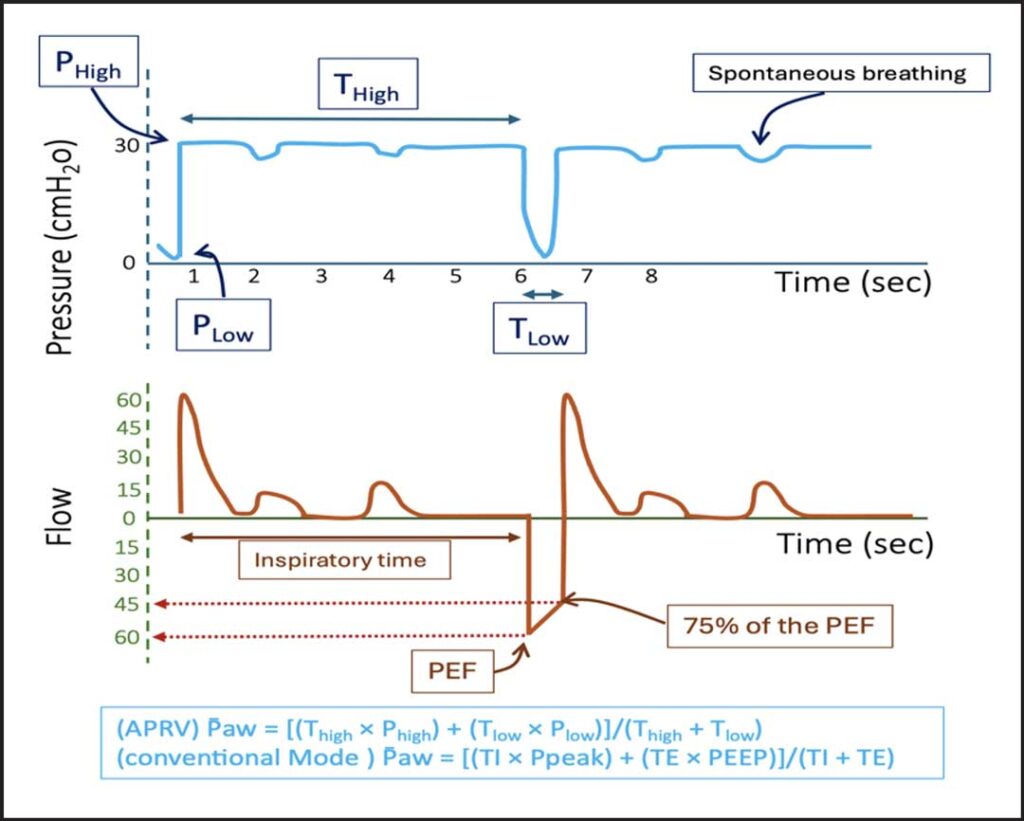
Airway pressure release ventilation (APRV), first described in 1986, was developed as an alternative mode of mechanical ventilation to improve oxygenation while minimizing the risk of VILI.2 APRV reduces mechanical power by limiting repetitive high-pressure and high-volume cycles. It maintains a continuous high airway pressure (Phigh) for a prolonged period (Thigh) to keep alveoli open, with brief pressure releases (Plow) over a short time (Tlow) to allow partial exhalation.4–5 This results in an inverse I:E ratio. The Time-Controlled Adaptive Ventilation (TCAV) approach relies on correct APRV settings to promote lung recruitment and stabilization. One key aspect of TCAV is adjusting Tlow to terminate when 75% of the peak expiratory flow (PEF) is reached.5 This strategy helps prevent alveolar collapse and supports more effective ventilation and gas exchange (Fig 1).5–6

An important physiological advantage of APRV is its ability to generate a higher mean airway pressure (P̄aw) compared with conventional ventilation.7 This is achieved primarily through the prolonged duration at Phigh and the short release phase (Tlow), which together enhance alveolar recruitment and oxygenation at similar peak pressures. The extended Thigh also allows more time for gas mixing, which may reduce dead space and improve CO₂ clearance. However, while higher P̄aw can improve oxygenation, it may also reduce venous return and cardiac output—potentially impacting systemic oxygen delivery.7
Another important feature of APRV is its support for spontaneous breathing throughout the ventilation cycle. This can help maintain diaphragm activity and reduce the risk of ventilator-induced diaphragm dysfunction, while also improving patient comfort and synchrony (Fig 1).
Despite its potential benefits, APRV is not without risks. When used incorrectly or in patients who are not appropriate candidates, APRV can cause significant harm. Inappropriate settings—particularly an excessively long Tlow or overly high Phigh—can result in lung overdistention, hemodynamic compromise, or insufficient CO₂ clearance.
To date, two large studies have evaluated the early use of TCAV-APRV in ARDS, including a physiological comparison with low tidal volume (LTV) ventilation.5–9 Early application of APRV was associated with fewer ventilator days, reduced sedation requirements, and improved oxygenation.5 These benefits are believed to result from better patient comfort and the ability to breathe spontaneously, which promotes further alveolar recruitment and lung stabilization during Phigh, thereby reducing atelectotrauma.5,8
A recent study published in the journal CHEST® by Zou and colleagues further compared APRV and LTV ventilation using electrical impedance tomography.8 This study found that APRV led to improved dorsal lung recruitment, better V̇/Q̇ matching, and superior oxygenation.
In conclusion, APRV has traditionally been viewed as a salvage therapy in patients with ARDS. However, more recent literature suggests that TCAV-APRV can provide better overall lung recruitment with less sedation and more ventilator-free days. Knowing this, APRV may be something that clinicians utilize in early ARDS care.
References
1. von Düring S, Parhar KKS, Adhikari NKJ, et al. Understanding ventilator-induced lung injury: the role of mechanical power. J Crit Care. 2025;85:154902. doi:10.1016/j.jcrc.2024.154902
2. Beitler JR, Malhotra A, Thompson BT. Ventilator-induced lung injury. Clin Chest Med. 2016;37(4):633-646. doi:10.1016/j.ccm.2016.07.004
3. Stock MC, Downs JB, Frolicher DA. Airway pressure release ventilation. Crit Care Med. 1987;15(5):462-466. doi: 10.1097/00003246-198705000-00002
4. Jain SV, Kollisch-Singule M, Sadowitz B, et al. The 30-year evolution of airway pressure release ventilation (APRV). Intensive Care Med Exp. 2016;4(1):11. doi:10.1186/s40635-016-0085-2
5. Cheng J, Ma A, Dong M, et al. Does airway pressure release ventilation offer new hope for treating acute respiratory distress syndrome? J Intensive Med. 2022;2(4):241-248. doi:10.1016/j.jointm.2022.02.003
6. Chatburn RL, Volsko TA. Documentation issues for mechanical ventilation in pressure-control modes. Respir Care. 2010;55(12):1705-1716.
7. Spinelli E, Mauri T, Beitler JR, Pesenti A, Brodie D. Respiratory drive in the acute respiratory distress syndrome: pathophysiology, monitoring, and therapeutic interventions. Intensive Care Med. 2020;46(4):606-618. doi:10.1007/s00134-020-05942-6
8. Zou X, Zhang H, Wu Y, et al. Physiologic comparison of airway pressure release ventilation and low tidal volume ventilation in ARDS: a randomized controlled trial. Chest. 2025;167(2):453-465. doi:10.1016/j.chest.2024.08.050
9. Zhou Y, Jin X, Lv Y, et al. Early application of airway pressure release ventilation may reduce the duration of mechanical ventilation in acute respiratory distress syndrome. Intensive Care Med. 2017;43(11):1648-1659. doi:10.1007/s00134-017-4912-z
