As CHEST gathers for its annual meeting in Chicago, it is also highlighting critical services provided by three local health groups and supporting their programs through CHEST Community Connections.
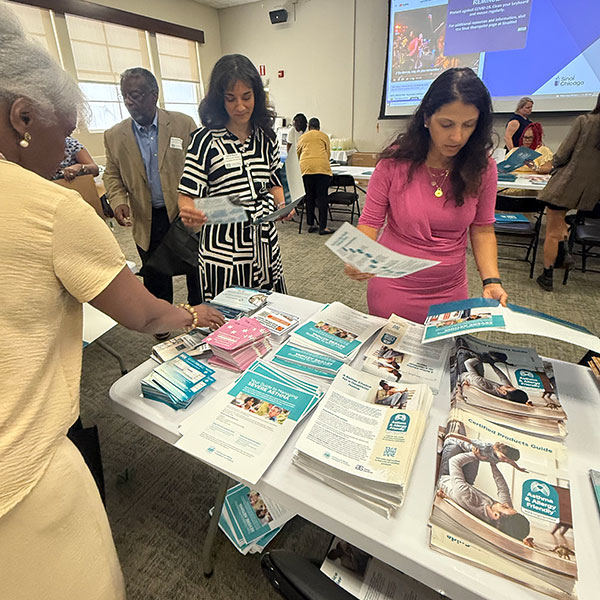
Now in its third year, the Community Connections initiative partners with selected nonprofits in the host city of the CHEST Annual Meeting. For the 2025 meeting in Chicago, CHEST is working with the Chicago Asthma Consortium, CommunityHealth, and Mobile Care Chicago. Each organization has received an unrestricted grant of $5,000 and has been given a platform in the Exhibit Hall to inform attendees about their work.
Elizabeth Stigler, PhD, who coordinates the project in her role as CHEST’s Director of Diversity, Equity, Inclusion, and Belonging, describes the Community Connections initiative as the organization’s commitment to transformative, community-led support.
“We feel it is important to meaningfully contribute to the site of our annual meeting, and we want to do that beyond just coming in for four to five days and just doing one thing such as cleaning a beach or a park,” Dr. Stigler said. “We recognize there are client-facing organizations on the ground and connected to their patients and communities. They have those relationships, they understand the landscape of need, and they know the state of public and community health in their cities better than we do.”
The community support also includes a premeeting off-site volunteer activity for CHEST leadership. This year’s activity will be with the Chicago Asthma Consortium on the Saturday preceding the meeting.
Dr. Stigler described the event and the broader goal of the Community Connections program as a two-way partnership, noting that CHEST members might be able to take away actionable ideas from their encounters with the Chicago nonprofits.
“It offers a knowledge-transfer opportunity,” Dr. Stigler said. “The initiatives, strategies, and services that these organizations employ might be novel, innovative, and something that our attendees might be able to take back to their own patients or communities.”
How to Meet the Groups
The three Community Connections partner groups have been invited to present information about their missions and work from 11:15 am to 12 pm CT on Tuesday, October 21, at Experience CHEST in the Exhibit Hall. Group representatives will also attend the Cultures and Communities Reception, which begins at 6 pm on Monday, October 20, on Level 33 of the Marriott Marquis.
Chicago Asthma Consortium
Asthma is a disease of disparity.
The chronic lung condition affects nearly 25 million Americans, but the burden of asthma “falls disproportionately on racial and ethnic minority populations,” according to a 2020 Asthma and Allergy Foundation of America report.
These disparities are particularly pronounced in Chicago, which a 2020 study by the University of Illinois, Chicago, characterized as “an epicenter for asthma-related health inequities affecting children in the United States.”
Founded in 1996, the Chicago Asthma Consortium (CAC) is marking three decades of working to overcome these disparities through educational programs and community involvement. The group supports a range of in-person and virtual educational events, including webinars, lunch-and-learns, conferences, and community gatherings to bridge researchers, experts, patients, and community members so that they can learn from one another.
“As a community-based organization, we have the privilege of connecting with a diverse group of partners who are passionate about the fight against asthma,” said CAC Executive Director Rachelle Paul-Brutus, MPH. “These partners include health practitioners, nurses, community health workers, researchers, respiratory health therapists, pharmacists, leaders from community-based organizations, asthma stakeholders, and community members who can tell us their lived experience with asthma and inform the type of work that is important to them.”

When you think about asthma, you realize it is not a fight for one person or one group alone, Paul-Brutus said. “Asthma is an illness that requires all hands on deck. It requires working in partnership, in a consortium, to have different perspectives and different feedback to be successful.”
Paul-Brutus emphasized that having a community-centered approach allows for information and conversations to reflect the varied realities and concerns of each community.
“We have such different neighborhoods and communities that we cannot have a one-size-fits-all approach to the issue,” she said. “We need to be intentional about addressing the disparities. Depending on where you live in Chicago, for example, the air quality is not the same. You have some neighborhoods close to industrial corridors and others close to nature. One neighborhood is close to a park and another is close to a railroad track. Your approach to asthma in Lincoln Park, for example, is not going to be the same as your approach in the southeast side of Chicago.”
Paul-Brutus said that in some areas, residents must choose between paying their rent or purchasing asthma medication. Understanding the socioeconomic realities on the ground and being connected to neighborhoods through community advisory panels better allows the CAC to develop specific priorities for each region. One neighborhood might prioritize seminars on indoor air quality, another might need to focus on primary care options, while a third might find that advocating for different zoning laws to improve air quality might make the most significant impact.
Paul-Brutus, who worked in research and public health for more than 20 years, acknowledged that nonprofit health groups are increasingly facing challenges. But, she added, it is important to retain access to the latest data and studies to stay current on the different realities that affect communities. It is essential to remember that numerous studies have shown the disparities in asthma—how socio-economic conditions and implicit or explicit racism lead to different risks and rates of asthma in different neighborhoods, she said. And it is important to recognize how changes in personal habits, communities, and policy can improve individual and community health.
“We have a solid foundation,” Paul-Brutus said. “The data we receive from the city, the county, and the state show the disparities of asthma, but it also gives me hope and the strength to keep going, regardless of the situation we live in. We want to make sure that we continue to impact lives—this is too important to stop.”
Lend a Hand at CHEST 2025
CHEST 2025 attendees will have the opportunity to participate in a service event with Chicago nonprofit Envision Unlimited on Sunday, October 19, at the McCormick Place Convention Center.
For more than 75 years, Envision Unlimited has served people living with intellectual and developmental disabilities by providing empathetic care and services that promote independence and inclusion. The program currently supports 5,000 members of all ages in the Chicago area and Central Illinois, regardless of race, gender, religion, or ability to pay.
Beginning at 9:45 am CT on Sunday, all CHEST 2025 attendees are invited to help put together care kits for Envision Unlimited members who are entering community living or foster care. Meeting attendees can also write personalized letters of support. The service event will take place near the main registration area of the convention center and last until 2:45 pm or until all 500 kits are complete.
CommunityHealth
The mission of CommunityHealth is both unique and simple, according to Alice Woo, the Chicago nonprofit’s Funder and Donor Relations Manager.
“We are one of the largest volunteer-based clinics in the country, and we serve uninsured patients,” Woo explained. “We don’t do any insurance billing—no reimbursement model. We simply provide the care with no charge to the patient.”
CommunityHealth was founded in 1993, when the late Serafino Garella, MD, then an internist, organized a group of young, like-minded colleagues to survey the health care needs of Chicago communities. After discovering that nearly half the people they talked to lacked insurance or a consistent medical provider, Dr. Garella secured funding and support from others to operate a free walk-in clinic twice a week.
More than 30 years later, the program has expanded to a full-service volunteer clinic—with an in-house pharmacy—and more than 20 specialties, including dental, sleep, behavioral health, cardiology, nephrology, and physical therapy. In addition, the clinic operates three microsites across Chicago.

Woo said that CommunityHealth’s expansion has relied on key concepts that have always defined the clinic, including the cultivation of long-term partnerships and a deep network of volunteer professionals.
Two behavioral health counselors, a dentist, a director of clinical operations, and a nurse practitioner constitute the clinic’s entire full-time staff. Volunteers provide all other medical services.
Those volunteers include retired, midcareer, and early career professionals, as well as medical students and residents.
Currently, CommunityHealth works with 16 academic institutions throughout Chicago, such as the University of Chicago, Loyola University Stritch School of Medicine, Rush University College of Nursing, Northwestern University, the University of Illinois, Chicago, and others, whose students and residents provide a dependable way to staff clinics.
“And some of these volunteers stick around for decades,” Woo added. “We have some amazing folks who have given over 1,000 hours.”
One former volunteer who made a significant impact at CommunityHealth is Justin Fiala, MD, an ICU physician and sleep medicine specialist who volunteered as a student at the University of Illinois, Chicago, and later returned to Chicago as an Assistant Professor at Northwestern University’s Feinberg School of Medicine.
Dr. Fiala reunited with CommunityHealth in 2021, when the clinic was recognizing a need for a sleep clinic.
“Patients were expressing fatigue,” Woo explained. “One patient talked about how he was falling asleep behind the wheel, and a lot of patients were suffering from sleep apnea. But we didn’t have a program to make those treatments happen. We were applying for donations of CPAP machines on an individual patient basis.”
Dr. Fiala helped establish a sleep clinic at CommunityHealth backed by a grant from Northwestern and the American Academy of Sleep Medicine Foundation. He also spearheaded an initiative to secure donated CPAP machines and begin printing customized CPAP masks courtesy of a 3D printer made available by Northwestern.
Woo described these actions as a unique success story that is also emblematic of the patient-centered approach CommunityHealth strives to take throughout its clinic.
“The sleep clinic is just one of the ways we try to provide individualized care and make each patient feel like they have a care team supporting them,” Woo said. “For example, if a patient is diagnosed with diabetes, then they would immediately have access to podiatry, endocrinology, nephrology, ophthalmology, and a dietician, if needed, plus priority dental care screening.”
In recent years, this comprehensive approach has expanded to include community workshops and classes on themes from diabetes, hypertension, women’s health, and home health hazards. That last workshop includes follow-up actions such as providing hypoallergenic pillowcases and even sending in renovators to insulate windows or to improve ventilation in a home or apartment.
Woo said each of these initiatives is guided by partnerships with community organizations working from within the cultural context of the neighborhoods and often through language interpretation, with Spanish and Polish being the most in-demand.
While the political landscape and challenges to traditional funding have forced CommunityHealth to rethink some of its models, Woo said it was important to point out the net benefits of nonprofit clinics and community networks.
“Part of the strength of these partnerships is the understanding that CommunityHealth’s work in preventive care and [part of] consistent care for uninsured people is preventing ER visits,” Woo said. “It’s estimated that we save local emergency rooms around $9 million per year just by preventing emergency situations and conditions from getting too far along.”
Connections for 2026 (and Beyond)
Do you know a nonprofit group doing amazing work for respiratory health in Phoenix, the host city of CHEST 2026? Or maybe you know of a group doing extraordinary work in Vancouver, Canada, the host city of CHEST 2027? If so, you can nominate the group for a CHEST Community Connections grant online at info.chestnet.org/community-connections.
Mobile Care Chicago
In 1998, four local physicians teamed up to counteract geographic health disparities in Chicago by focusing on areas that had abnormally high asthma mortality rates. This collaboration led to the formation of Mobile Care Chicago (MCC), and in 1999, the group launched its first Asthma Van, an RV transformed into a clinic on wheels, providing care for kids in Chicago neighborhoods with high asthma rates.
With the support of a CHEST grant in 2000, MCC was able to deliver free medical and preventative care to those without access in their own communities.
“CHEST helped to launch us into the mobile care we are today,” said Executive Director Matt Siemer.

Twenty-five years later, MCC now has a fleet of six mobile units, which includes three asthma and allergy mobile clinics, plus vans for dental, vision, opioid recovery, and food allergies.
Each van, uniquely painted by local artists, is equipped with a mobile unit—a nurse practitioner or medical doctor, a nurse, a medical assistant, and a clinical technician who also serves as the van’s driver—with the goal of diagnosing, educating, and providing ongoing care for kids.
“When kids are sick or struggling to breathe at night, worried parents and the entire household don’t get much sleep,” said Melinda Fitzgerald, PNP, MCC’s Clinical Compliance Lead. The child’s health, the parents’ work life, and the student’s school attendance are all affected, which then affects the surrounding community.
To keep care convenient for working parents, MCC partners with 60 Chicago Public Schools and 25 Lake County schools, giving greater access to interface with health professionals like school nurses, Siemer said. Appointments are year-round and open to all kids, even if they do not attend the school where the one of the vans is visiting.
At every Asthma Van appointment, a team member checks the patient’s vitals and conducts an asthma diagnostic test, a spirometry test, and a fractional exhaled nitric oxide (FeNO) test, if necessary. In another area, a team member reviews the patient’s history with the parent. Once all the information is gathered, the care team devises a treatment plan. The team works with the parents, the child, and the school to ensure everyone is educated about the child’s condition(s) and medication(s).
A second Community Impact Grant from CHEST in 2018 helped expand this program to explore social determinants of health—like environmental factors, substandard housing, air quality, and mental health—and their correlation to patient care.
“Every time that we’ve had a significant new expansion or innovation, CHEST is always there alongside it,” Siemer said.
And patients stick around, too. A Community Impact Grant that MCC received from CHEST in 2024 enhanced the organization’s ability to serve the young adult population (ages 16+) who have been coming to the Asthma Van since they were kids.
“Now, 10% of our patient population fits the young adult category, and next year it’s going to be 12%,” Siemer said. “As our Asthma Van patients age, they turn from children into young adults into adults who have a new perception of what health care can be—an alternative to institutional medicine.”
Siemer noted that many of these patients have grown up using mobile health care and now bring their own kids for mobile care and spread the word to their neighbors.
“Parents, people in schools, primary care providers—there’s a whole host of people who are all stakeholders in a child’s health,” Siemer said. “We are counselors, and we can give advice based on best practices and evidence, but we alone cannot facilitate change. Asthma is a contextual disease, and it takes a community effort. Our Asthma Van can get you thinking about care in a different way.”
Note: This section on Mobile Care Chicago originally appeared as a longer story, “Where the Rubber Meets the Remedies,” by Morgan Lord in CHEST Advocates. It is adapted and reprinted with permission.
Enduring Encounters
Continuing impact from Boston, Honolulu meetings
One of the goals of the Community Connections initiative is to create enduring encounters between CHEST and the host city organization partners. Elizabeth Stigler, PhD, who coordinates the project in her role as CHEST’s Director of Diversity, Equity, Inclusion, and Belonging, noted that both the 2023 program in Hawai‘i and the 2024 program in Boston created meaningful follow-up opportunities.
After CHEST partnered with Waianae Coast Comprehensive Health Center during CHEST 2023 in Honolulu, the center reached out to CHEST Advisory Board Member Burton Lesnick, MD, FCCP, to request a special video presentation from the expert on pediatric pulmonology for their pulmonology team.
When CHEST worked with Boston Health Care for the Homeless Program as a Community Connections partner during CHEST 2024, the organization helped educate CHEST members and leadership about their nonstigmatizing approach to providing services for the unhoused community.
“That helped us become aware of some of the research, particularly around the presence of stigmatizing language in the care for sepsis patients leading to adverse outcomes, or how stigmatizing language around substance use and abuse can prevent people from seeking appropriate care,” Dr. Stigler said.
CHEST applied this information to help develop a new First 5 Minutes®: Patient-Centered Approaches to Critical Care—which will launch in the coming months—and tapped one of the Boston Health Care for the Homeless Program as a core faculty member in developing that module.
“So, we’re continuing our relationships,” Dr. Stigler said. “We’re continuing to bring expertise and education that we learned from our community partners and to incorporate that into our education at CHEST.”
Call for Topics Is Open
Feeling inspired by all the great sessions in Chicago? Help shape the curriculum for CHEST 2026, October 18 to 21 in Phoenix, by submitting topic ideas from areas you’re passionate about, topics affecting your practice, or new technologies you’d like to learn more about. The submission deadline is Tuesday, December 2, at 2 pm CT.