
Mechanical ventilation is a lifesaving intervention used to support patients with respiratory failure. However, improper settings can lead to complications, such as diaphragm dysfunction.1 This can occur due to ventilator overassistance, ventilator underassistance, or eccentric loading of the diaphragm. Excessive unloading of the diaphragm from overassistance can reduce inspiratory effort, resulting in disuse atrophy.2,3 Conversely, excessive loading of the diaphragm from underassistance can cause acute muscle inflammation and injury, also known as underassistance myotrauma.4–7 While lung-protective protocols are routinely implemented, the concept of diaphragm-protective ventilation has recently emerged as a valuable and complementary strategy to mitigate the risk of diaphragm dysfunction.1
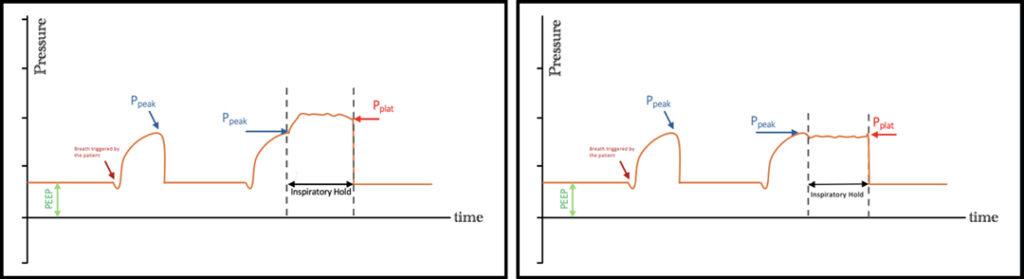
Various techniques, such as diaphragm ultrasound, esophageal manometry, and diaphragm electrical activity, can assess patient respiratory effort (Pmus) to set optimal ventilator settings for diaphragm protection, but they require additional equipment and specialized training.1,8 This review emphasizes a practical, feasible, and noninvasive approach using mechanical ventilator graphics to monitor Pmus. By performing a brief end-inspiratory occlusion maneuver, reliable plateau pressure (Pplat) measurements can be obtained, even during assisted ventilation.9 This method is valuable for assessing Pmus and to ensure proper ventilator settings. During an inspiratory occlusion maneuver, inspiratory muscles relax, resulting in increased airway pressure (Paw). If Pplat exceeds peak pressure (Ppeak), it may indicate that the patient is making vigorous Pmus. This situation occurs when the patient’s respiratory muscles contribute to lung inflation in addition to the positive pressure generated from the ventilator (Figure 1a).7,10 In contrast, minimal difference between Ppeak and Pplat signifies minimal Pmus (Figure 1b). This maneuver helps assess respiratory muscle activity and determine the level of assistance needed.

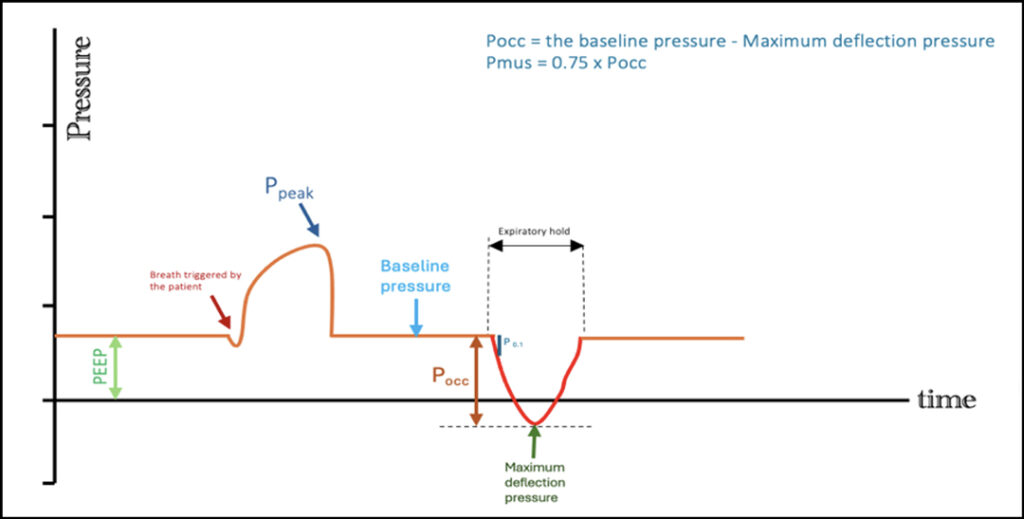
A brief expiratory occlusion can also be used to evaluate Pmus. By performing an expiratory hold, any inspiratory muscle activity will create negative pressure, which can be observed as a decrease in Paw. Airway occlusion pressure is the decrease in Paw during the first 100 milliseconds after the onset of inspiration and is a reliable measure of excessive inspiratory drive (ref, 1-3.5 cm H20).8 In addition, the maximum pressure deflection at end-expiratory generated by the patient’s respiratory effort against an occluded airway (Pocc) represents the pressure produced by the respiratory muscles to expand the lungs and chest wall during mechanically assisted breaths. This measurement can be used to assess excessive Pmus (Figure 2).7,11 Pmus is approximately two-thirds of Pocc. Maintaining Pmus between 5 to 10 cm H2O helps prevent both overassistance and underassistance diaphragmatic myotrauma.11
In conclusion, personalizing mechanical ventilation settings is essential for protecting the lungs and diaphragm. Utilizing mechanical ventilator graphics to monitor Pmus is a practical, reliable, and noninvasive approach for effective ventilation management. This technique enables health care professionals to ensure proper ventilator settings, minimize complications, and improve patient outcomes.
References
1. Goligher EC, Jonkman AH, Dianti J, et al. Clinical strategies for implementing lung and diaphragm-protective ventilation: avoiding insufficient and excessive effort. Intensive Care Med. 2020;46(12):2314-2326.
2. Goligher EC, Dres M, Fan E, et al. Mechanical ventilation-induced diaphragm atrophy strongly impacts clinical outcomes. Am J Respir Crit Care Med. 2018;197(2):204-213.
3. Demoule A, Jung B, Prodanovic H, et al. Diaphragm dysfunction on admission to the intensive care unit. Prevalence, risk factors, and prognostic impact-a prospective study. Am J Respir Crit Care Med. 2013;188(2):213-219.
4. Levine S, Nguyen T, Taylor N, et al. Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans. N Engl J Med. 2008;358(13):1327-1335.
5. Dres M, Goligher EC, Heunks LMA, Brochard LJ. Critical illness-associated diaphragm weakness. Intensive Care Med. 2017;43(10):1441-1452.
6. Hooijman PE, Beishuizen A, Witt CC, et al. Diaphragm muscle fiber weakness and ubiquitin-proteasome activation in critically ill patients. Am J Respir Crit Care Med. 2015;191(10):1126-1138.
7. Goligher EC, Dres M, Patel BK, et al. Lung- and diaphragm-protective ventilation. Am J Respir Crit Care Med. 2020;202(7):950-961.
8. Telias I, Junhasavasdikul D, Rittayamai N, et al. Airway occlusion pressure as an estimate of respiratory drive and inspiratory effort during assisted ventilation. Am J Respir Crit Care Med. 2020;201(9):1086-1098.
9. Bellani G, Grassi A, Sosio S, et al. Driving pressure is associated with outcome during assisted ventilation in acute respiratory distress syndrome. Anesthesiology. 2019;131(3):594-604.
10. Sajjad H, Schmidt GA, Brower RG, Eberlein M. Can the plateau be higher than the peak pressure? Ann Am Thorac Soc. 2018;15(6):754-759.
11. Bertoni M, Telias I, Urner M, et al. A novel non-invasive method to detect excessively high respiratory effort and dynamic transpulmonary driving pressure during mechanical ventilation. Crit Care. 2019;23(1):346.