
Mechanical power (MP) is the measure of the total energy delivered to the respiratory system over time, typically expressed in joules per minute (J/min). This energy dissipation within the lungs can lead to inflammation and disruption of cells and the extracellular matrix, culminating in ventilation-induced lung injury and worse outcomes, including higher mortality and prolonged mechanical ventilation.1
MP integrates the effect of tidal volume, airway pressure (including driving and peak pressure), flow, and respiratory rate, quantifying the contribution of respiratory rate and the positive end-expiratory pressure to the total power delivered by the ventilator. MP-based strategies aim to minimize unnecessary power delivery and reduce harm. Mathematically, the power equation is derived from the equation of motion multiplied by the changes in lung volume and respiratory rate.1–2
Can MP be reliably measured at the bedside?
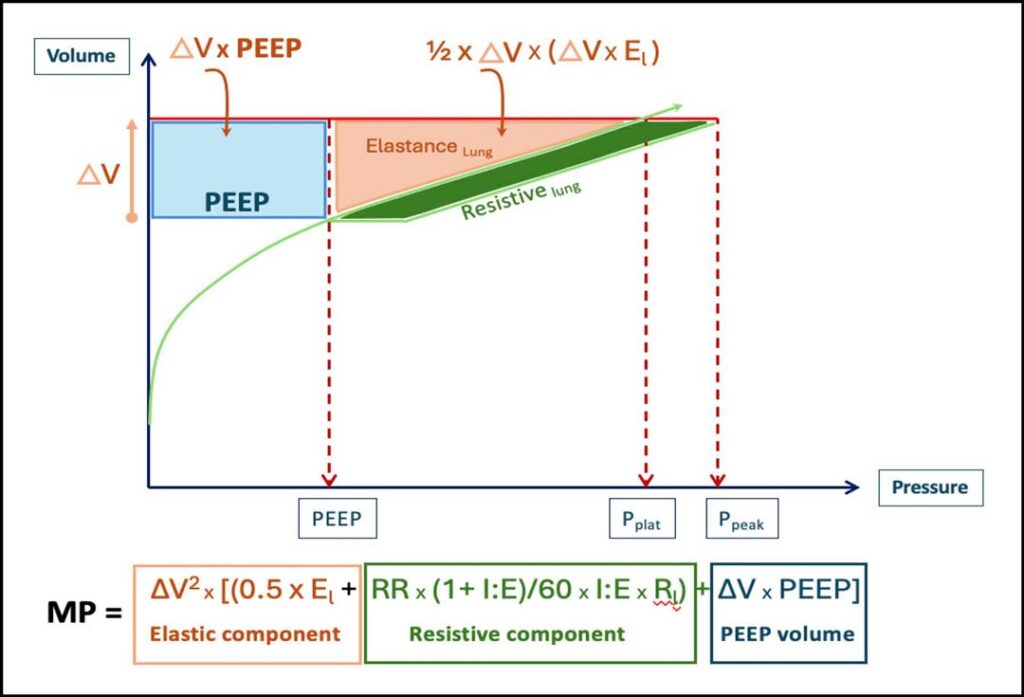
MP can be estimated using two main approaches: a direct measurement (geometric method) or calculation through equations.3 The geometric method measures MP as the area under the inspiratory limb of the airway pressure-volume curve (see Figure 1), expressed in joules and multiplied by the respiratory rate (J/min). While accurate, this method is rarely practical in routine care.
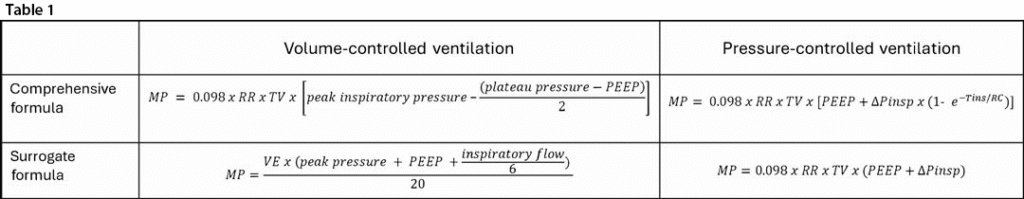
Alternatively, MP can be calculated using mode-specific formulas (see Table 1). The comprehensive equation offers greater precision, and the surrogate formula is for bedside simplicity, but both offer good approximation for clinical use.3

Should MP replace traditional targets like plateau pressure and driving pressure?
MP is an appealing concept but its implementation in daily clinical decision-making imposes some challenges. Manual calculation can be cumbersome and difficult to integrate into routine workflows, as well as not universally applicable across ventilation modes.
However, the optimal threshold for safe mechanical power and its routine use in guiding ventilation strategies remains an area of ongoing research. A threshold of > 18 J/min was shown to correlate with increased mortality, and cumulative exposure above this threshold was associated with increased probability of death in the ICU.4
Current best practice should aim to incorporate MP as an adjunct to traditional targets, when possible, since it integrates components of ventilation that may also contribute to lung injury and should not be overlooked. Attention to possible breath-to-breath variation in power should also be considered.
How might targeting MP influence ventilator strategies based on patient-specific characteristics?
When implementing MP in clinical practice, it is important to consider the variability in pathology and patient characteristics to help guide your ventilation strategy. The same MP may produce different physiological consequences depending on individual factors (ie, healthy or injured lungs).2 Several approaches have been explored to personalize MP. Strategies such as normalization of MP to ideal body weight involve real-time adjustment of tidal volume, respiratory rate, PEEP, respiratory system compliance, or CT-proportion of well-inflated lungs have been explored to minimize energy delivery while maintaining adequate gas exchange.5–6 The recently introduced concept of MP ratio further acknowledges the importance of individualized ventilation strategies rather than a one-size-fits-all target.7
References
1. Tonetti T, Vasques F, Rapetti F, et al. Driving pressure and mechanical power: new targets for VILI prevention. Ann Transl Med. 2017;5(14):286. doi:10.21037/atm.2017.07.08
2. Gattinoni L, Collino F, Camporota L. Mechanical power: meaning, uses and limitations. Intensive Care Med. 2023;49(4):465-467. doi:10.1007/s00134-023-06991-3
3. Chiumello D, Gotti M, Guanziroli M, et al. Bedside calculation of mechanical power during volume- and pressure-controlled mechanical ventilation. Crit Care. 2020;24(1):417. doi:10.1186/s13054-020-03116-w
4. Manrique S, Ruiz-Botella M, Murillo N, et al. Impact of mechanical power on ICU mortality in ventilated critically ill patients: a retrospective study with continuous real-life data. Eur J Med Res. 2024;29(1):491. doi:10.1186/s40001-024-02082-1
5. Zhang Z, Zheng B, Liu N, et al. Mechanical power normalized to predicted body weight as a predictor of mortality in patients with acute respiratory distress syndrome. Intensive Care Med. 2019;45(6):856-864. doi:10.1007/s00134-019-05627-9
6. Coppola S, Caccioppola A, Froio S, et al. Effect of mechanical power on intensive care mortality in ARDS patients. Crit Care. 2020;24(1):246. doi:10.1186/s13054-020-02963-x
7. D’Albo R, Pozzi T, Nicolardi RV, et al. Mechanical power ratio threshold for ventilator-induced lung injury. Intensive Care Med Exp. 2024;12(1):65. doi:10.1186/s40635-024-00649-0
