Lactation is not a topic that most intensivists study deeply. But lactation—or the lack thereof—is a key issue for new mothers in the ICU and their newborns.

“Being in the ICU can be very traumatizing for patients, and this is compounded when they are separated from their new infant,” said Kayla Kolbe, MD, Clinical Assistant Professor of Pulmonary and Critical Care Medicine at the University of Michigan Medical School. “Lactation in a critically ill person can be a bridge between the patient and the separated infant—a way to parent from afar. At a time when much is going wrong, lactation is something that can go right.”
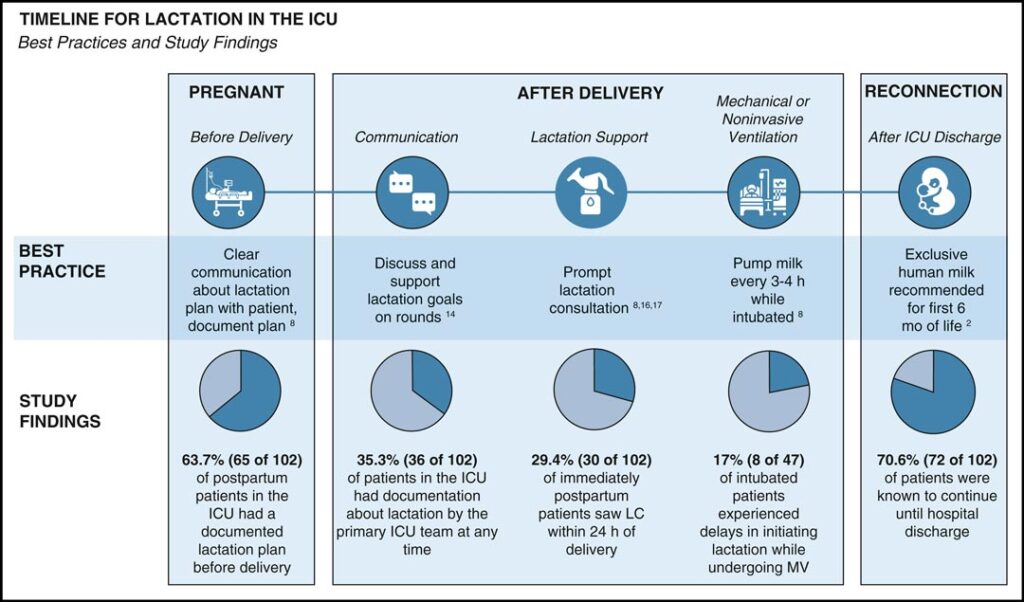
Dr. Kolbe is lead author on Lactation Practices in Critically Ill Patients, what may be the first systematic attempt to explore lactation practices and barriers in ICU patients. A retrospective chart review of patients who are immediately postpartum in the ICU at an academic medical center between January 2018 and January 2024 found that most new mothers in the ICU (85%) initiated lactation with about 70% continuing until hospital discharge.
But lactation in the ICU lagged the rate of initiation in the general US population. And despite widespread guidelines recommending extended breastfeeding, there are few guidelines on lactation in critically ill patients.

“There has been a massive growth of information [on] and appreciation of human milk biology and the positive role human milk plays in the health of the newborn and mother,” said Michael Marll, MD, Pulmonary and Critical Care Fellow at Emory School of Medicine.
“When it comes to translating that knowledge into practice, there have been many unknowns,” Dr. Marll said. “What is fascinating about this article is that it provides a framework to address the barriers to successful lactation in [critically ill patients] and improve our support in shared decision-making with families.”
Key among the recommended best practices outlined in the paper are clear communication about lactation plans and discussion and support of lactation goals. Other best practices include prompt lactation consultation and regular expression of breast milk for patients who are intubated (see diagram).
Lack of knowledge is a key barrier, Dr. Kolbe said. Lactation is rarely discussed during intensivist training or on rounds. ICU teams may not recognize the importance of lactation in the rush to admit a critically ill patient.
“There is also this notion, this question, of whether it is physiologically harmful for somebody to lactate during critical illness,” she said. “Is lactation contraindicated in critical illness? Absolutely not. Is it even possible for the critically ill body to lactate? It is. Lactation is a biologically driven process that happens whether you’re critically ill or not. It’s just a matter of whether you support the continuation of lactation.”
Reprinted with permission from CHEST® Critical Care.
Research found that patients who have a documented plan to lactate when they enter the ICU are more likely to continue, Dr. Kolbe said. Patients or caregivers who met with a lactation consultant during the admission were also more likely to continue lactation.
Mechanical ventilation and aggressive medication use should not delay initiating lactation, she added. Breast pumps are appropriate for patients who are awake or sedated, but milk expression must begin early and continue on a regular basis to establish and preserve milk supply once the illness resolves.
“We can improve our practices for patients who may not have had prior plans,” Dr. Marll said. “Those early hours immediately after delivery are incredibly important to the establishment of milk production.”
Delay in initiation or failure to maintain consistent attempts at milk expression can inhibit future milk production, as lactocytes can atrophy from disuse, he added.
“Patients feel so strongly about lactation, even in the face of life-threatening critical illness. The documentation of their feelings and experiences just screamed out at us so powerfully from the charts,” Dr. Kolbe said. “If intensivists were aware of this importance, they would be more in tune with communicating about lactation and protecting it. This is a way we can help empower patients during critical illness.”
